Bone marrow transplantation is a medical procedure that replaces damaged or destroyed bone morrow resulting from primary or secondary infiltrative diseases, infections, or chemotherapy, with healthy bone marrow stem cells.
The transplanted new stem cells produce new blood cells and promote the growth of new bone marrow.
Chemotherapy, radiation or both may be given prior to transplantation. This may be done with high doses of chemotherapy, radiation or both (ablative treatment), or lower doses of chemotherapy, radiation or both (reduced intensity treatment or mini transplant).
There are three kinds of bone marrow transplants that consist of autologous bone marrow transplant, allogeneic bone marrow transplant, and umbilical cord blood transplant. Bone marrow transplant is performed on children and adults.
Bone marrow transplantation is a serious surgical procedure that is expected to be a permanent solution in the treatment of many diseases. Bone marrow taken from a healthy individual is transplanted to the patient quickly and accurately. Bone marrow transplantation, which is performed by opening a vascular access, should be performed meticulously in hospitals, in extremely hygienic environments and using sterile instruments.
What is Bone Marrow Transplantation?
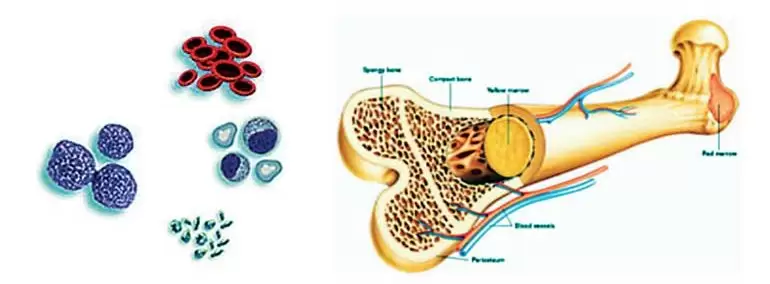
Marrow transplantation or bone marrow transplantation is a procedure performed to replace damaged or diseased cells in the bone marrow with healthy stem cells. Bone marrow is basically a spongy tissue that is responsible for the production of blood cells in the body. Marrow transplantation is usually used in the treatment of leukemia, lymphoma, aplastic anemia and some genetic diseases.
Bone marrow is found in the bone in both humans and animals and has a spongy structure. Thanks to the hematopoietic content in the bone marrow, it plays an important role in the transfer of cells called blood-forming stem cells. Thanks to these cells with the power of construction, it is possible to increase the body’s resistance against all kinds of disruptions in the body and to restructure itself.
Bone marrow transplantation can be defined as the process of replacing and renewing the bone marrow produced by the body’s blood cells with stem cells obtained from the patient’s own body or another person’s body in cases where it loses its function or cannot function due to various disorders. When the bone marrow is damaged due to various infections, blood cell-derived cancers, or chemotherapy for other reasons, the need for bone marrow renewal may arise.
In bone marrow transplantation, stem cells found in the bone marrow tissue and from which all blood cells originate are used. These cells, also known as hematopoietic stem cells; provide the formation of bone marrow tissue and the production of blood cells such as red blood cells, white blood cells and platelets.
How is Bone Marrow Transplantation Performed?
In order for bone marrow transplantation to be performed, there must be tissue compatibility between the patient and the donor. Tissue compatibility means that the antigens on the surface of the patient’s and donor’s blood cells are similar to each other. Antigens can be defined as molecules that allow the immune system to recognize foreign substances in the body. Tissue compatibility is important in terms of reducing the risk of the patient’s body rejecting donor cells.
Tissue compatibility is determined by the HLA test. For this, the patient’s and donor’s blood samples are examined in the laboratory. Although the most suitable donor for bone marrow transplantation may be the donor’s sibling or a close relative, this is not always possible. In this case, national or international stem cell donor registries can be used to find a suitable donor for the patient. These registries include the HLA types of volunteer donors. If a donor matching the patient’s HLA type is found, permission is requested from the donor for stem cell collection.
Stem cell collection can be done by bone marrow aspiration or peripheral blood stem cell collection. In the bone marrow aspiration method, bone marrow is taken from the donor’s hip bone or breast bone with a thin needle under local or anesthesia. The bone marrow taken from the donor is stored to be given to the patient.
In the peripheral blood stem cell collection method, the donor is given a drug that will allow the stem cells to pass from the bone marrow to the blood for a few days. The donor’s blood is taken with a needle connected to a machine. The stem cells are separated from the blood and the remaining blood is given to the donor. At the end of this process, which takes approximately 4 hours, the stem cells taken from the donor are stored to be given to the patient.
The process of giving stem cells to the patient is carried out like a blood transfusion. A tube is placed in the patient’s vein and the stem cells taken from the donor are transferred to the patient’s body through this. After the procedure, which takes about 1-2 hours, new blood cells begin to be produced as the stem cells reach the patient’s bone marrow. This process, called engraftment, is usually completed in 10 to 28 days. As a result of engraftment, the number of white blood cells increases first. This also means that the transplant produces new blood cells.
Marrow transplantation can be in the form of autologous or allogeneic marrow transplantation, depending on the compatibility of the patient and the donor tissue. In autologous marrow transplantation, the patient’s own stem cells are used. If the stem cells are not damaged by disease or treatment, bone marrow is taken from the umbilical cord blood or peripheral blood and frozen and stored. The bone marrow is killed with high doses of chemotherapy or radiotherapy. The purpose of this procedure is to destroy cancer cells in the patient’s body. After the procedure, the patient’s own stem cells are returned to the body.
In the allogeneic marrow transplantation method, the stem cells of a donor who is suitable for the patient are used. The patient’s sibling, relative or a registered donor can be the donor. By injecting stem cells from a donor into the patient’s body, it is possible to create a new immune system that can recognize and destroy the remaining cancer cells in the patient’s body. However, complications such as the patient’s body rejecting the donor cells or the donor cells attacking the patient’s body may occur.
In Which Diseases Is Bone Marrow Transplant Performed?
Bone marrow transplant is performed when the patient’s marrow is not healthy enough to function properly. This may be due to chronic infections, various diseases or cancer treatments. People with the following diseases may benefit from bone marrow transplant:
Acute leukemia
Aplastic anemia
Chronic leukemia
Hodgkin lymphoma
Myelodysplastic syndromes
Non-Hodgkin lymphoma
POEMS syndrome
Treatment-refractory or relapsed solid organ tumors
Adrenoleukodystrophy
Bone marrow failure syndromes
Hemoglobinopathies
Immune deficiencies
Multiple myeloma
Neuroblastoma
Plasma cell disorders
Primary amyloidosis
What are the Possible Complications Associated with Bone Marrow Transplant?
In allogeneic transplants, when the transplanted cells start to attack other cells in the body, grant versus host disease occurs. It can be defined as a complex clinical syndrome that results from organ dysfunction as a result of a severe immunological reaction mediated by healthy T-lymphocytes taken from the donor and given to the patient along with the stem cells. It is the most important cause of mortality and morbidity after allogeneic stem cell transplantation and can be seen immediately after transplantation or more than a year later.
There are two types of GVHD: acute and chronic. Acute GVHD usually occurs in the first months after transplantation and mostly affects the skin, liver or digestive system. Chronic GVHD can cause severe damage to many organs.
Signs and symptoms of chronic GVHD include joint or muscle pain, shortness of breath, persistent cough, vision changes, skin rashes, mouth sores, subcutaneous scarring or skin changes including hard skin.
What to Do Before Bone Marrow Transplantation?
A series of tests and procedures are performed to assess the patient’s general health and the donor’s condition, and to ensure physical readiness for the transplant. In addition, a surgeon or radiologist inserts an intravenous catheter, a long, thin tube, into a large vein in the chest or neck. This catheter usually remains in place during the treatment. This catheter, also called a central line, is used to infuse the transplanted stem cells, medications, and blood products into the body.
Working Hours
- Monday: 09:00 – 18:00
- Tuesday: 09:00 – 18:00
- Wednesday: 09:00 – 18:00
- Thursday: 09:00 – 18:00
- Friday: 09:00 – 18:00
- Saturday: 09:00 – 18:00
- Sunday: Closed
