Corneal transplantation, also known as keratoplasty, is a surgical procedure that replaces the degenerated or scarred corneal tissue with a healthy corneal tissue coming from a donor to restore glare and blurred vision problems, reduce pain and improve the appearance of the disordered cornea.
There are two main types of corneal transplants that are traditional full thickness corneal transplant, which is called penetrating keratoplasty (PK) and back layer corneal transplant which is called endothelial keratoplasty (EK).
As a result of various health problems encountered throughout life, different levels of damage may occur in body tissues or organs. Although there are various methods that can be applied for the treatment of organ failure, recently, tissue or organ transplantation from donor to recipient has been used as the main treatment for tissue and organ failure. In this context, corneal transplantation is among the methods applied for the renewal of corneal tissue, which is an important part of the eye.
What is Cornea Transplantation?
The transparent and dome-shaped tissue located at the very front of the eyeball is the cornea. The cornea, which provides the connection between the outside world and the eye, is the area where the light needed for the perception of the image is first transmitted to the eye and refracted. The light refracted by the cornea is refracted a second time by the lens of the eye after being transmitted to the inner part of the eye through the pupil and focuses on the macula, where clear vision occurs in the retina.
The image formed in the macula is transmitted to the nerve cells by the receptor cells and transmitted to the visual center of the brain and perceived. The cornea must be healthy in order for a clear image to be formed. The cornea tissue does not show direct blood supply, but instead obtains nutrients and oxygen through diffusion from the body fluid in the space between the cornea and the iris, the colored layer of the eye.
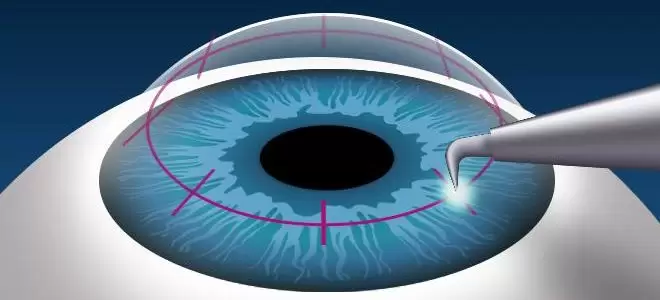
Removing the cornea whose structure has deteriorated due to various health problems affecting the cornea and transplanting the corneal tissue obtained from the donor to the patient is called cornea transplantation. In the cornea transplantation procedure, it is possible to transplant the entire corneal tissue or only its upper layer. In a small number of selected cases, artificial corneal tissues may be used in the transplantation process.
When is Cornea Transplantation Performed?
The cornea may be damaged due to injury, hereditary disease, infection, corneal degeneration and eye surgery complications. In this case, the diseased or damaged cornea may be replaced with a cornea taken from a healthy donor. Corneal transplantation can be performed in the following cases:
Corneal diseases
Corneal ulcers
Corneal injuries
Hereditary corneal disorders
Corneal transplantation is one of the most successful transplant surgeries. Today, corneal transplantation can be performed with the full-thickness, or penetrating keratoplasty, or half-thickness, or lamellar keratoplasty, depending on which corneal layer the disease in the corneal tissue affects.
Corneal transplantation is performed after the patient is given local or general anesthesia. The corneal tissue that has lost its transparency or shape is removed in full-thickness and the same size tissue prepared from the healthy donor cornea is transplanted to the patient. The donor cornea is sutured to the recipient cornea. The surgery is completed in approximately 45 to 60 minutes.
Today, corneal transplantation can be performed as full-thickness or half-thickness. In cases where the inner layer of the cornea, the endothelial layer, is healthy and the front layer is diseased, only the front layer of the cornea is replaced. The name of this surgical procedure is DALK, or Deep Anterior Lamellar Keratoplasty.
In cases where the corneal endothelial layer is insufficient, only this layer is replaced. For this, the Descemet Membrane Endothelial Keratoplasty (DMEK) method is applied. Although the success rate of this surgical procedure may vary depending on the patient, it is generally high.
In DALK surgery, the diseased front layer of the cornea is replaced, while the innermost layer, the endothelial cells, remain in place. Since the endothelial cells of the donor tissue are not removed, the risk of rejection of the transplanted cornea is greatly reduced.
In DMEK surgery, only the inner layer of the cornea is replaced, not the full layer. This method, which does not have many stitches, unlike full-thickness corneal transplantation, is called “sutureless corneal transplantation”. Since the front layer of the cornea is the patient’s own tissue, the cornea is much more resistant to trauma than a full transplant cornea.
What Methods Are Used in Corneal Transplantation?
Different methods and techniques can be used during corneal transplantation. In this context, the entire cornea or some of the corneal layers are replaced. Some of the basic methods used in corneal transplantation are as follows:
In the penetration (full) corneal transplantation method, the patient’s damaged corneal tissue is completely removed and the donor cornea is completely replaced. The donor cornea is fixed using stitches or tissue adhesives. Penetration transplantation provides a complete replacement of the corneal layers and renews all layers of the cornea.
The front layer (epithelial) transplantation method is performed by transplanting the epithelium, which is the surface layer of the cornea. In this method, which is used in some superficial corneal diseases, only the epithelium is replaced. Epithelial transplantation can provide an extremely fast healing process and improve visual function.
The middle layer (stroma) transplantation method is applied by transplanting the stroma, which is the middle layer of the cornea. Damaged or diseased stroma is removed and replaced with donor stroma. With lamellar stromal transplantation, only a portion of the corneal tissue is replaced, speeding up the healing process.
Donor Selection and Preparation in Cornea Transplantation
Donor selection and preparation are very important for the success of corneal transplantation. Donor selection should be meticulously performed to provide compatible and healthy corneal tissue. A cornea that maintains its optical transparency, is free of infection and has minimal pathological changes is considered an ideal donor cornea.
Donor cornea is usually obtained from brain-dead donors. Corneal banks play a critical role in collecting, processing, storing and allocating donor corneas to the appropriate recipient. Microbiological and histopathological tests are applied to evaluate the quality of donor corneas and determine their suitability. In this way, the risk of infection in the donor cornea can be reduced and transplant success can be increased.
Preparation of donor corneas is critical for achieving optimal transplantation results. Before corneal transplantation, the donor cornea is examined and cleaned. The corneal diameter and thickness are measured and cut to appropriate sizes if necessary. Before the transplant, the donor cornea is kept cold to preserve the vitality of the corneal cells and the healing process of the corneal tissue is supported during the transplant process.
Things to Consider After Corneal Transplantation
In order to support the healing process of patients after corneal transplantation and to achieve successful results, some factors should be taken into consideration. The most important of these is not to skip regular follow-up appointments. Thanks to these follow-ups, the doctor monitors the progress of the transplant and detects possible complications. During follow-up appointments, eye examinations, vision tests and necessary imaging techniques are used.
Another important point after corneal transplantation is the use of drugs that suppress the immune system to prevent rejection of the transplanted cornea. Regular and timely use of these drugs can ensure that the transplant is successful and the risk of regeneration is reduced.
It is extremely important for patients to pay attention to eye hygiene after corneal transplantation. Keeping the eyes clean reduces the risk of infection. At this stage, the eye drops recommended by the doctor should be used regularly and the eyes should be kept moist.
Wearing glasses or sunglasses is important in the period after corneal transplantation to provide adequate eye protection. This way, the eyes can be protected from damage that may be caused by external factors such as dust, wind or the harmful UV rays of the sun.
Working Hours
- Monday: 09:00 – 18:00
- Tuesday: 09:00 – 18:00
- Wednesday: 09:00 – 18:00
- Thursday: 09:00 – 18:00
- Friday: 09:00 – 18:00
- Saturday: 09:00 – 18:00
- Sunday: Closed
